6 May 2025
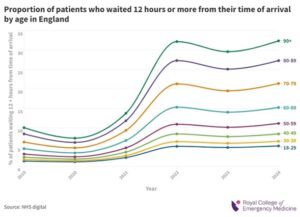
More than a million older people faced waits of 12 hours or more in A&Es in England last year – and shockingly, the older a person is, the more likely they are to experience a long stay in the ED – new data from the Royal College of Emergency Medicine (RCEM) reveals.
It comes as the College publishes a new report today (6 May 2025) looking at the care older people receive in Emergency Departments.
The research, titled ‘Care of Older People 2023-24’, is part of the College’s clinical Quality Improvement Programme which aims to improve the care of patients attending Emergency Departments. Today’s report reflects the findings of the second year of the three-year programme.
Across the UK, 149 Emergency Departments submitted 24, 865 patient cases from 4 October 2023 – 3 October 2024.
A key finding was that among patients over the age of 75, there was insufficient screening for three common conditions which primarily affect this age group.
It found:
Despite a year-on-year improvement from 2023, these patients are enduring the longest waits in A&Es and are bearing the brunt of an Urgent and Emergency Care system in crisis.
Older people are often more likely to suffer with complicated or multiple health issues. This, combined with the wider issues related to a shortage of in-patient beds, mean they can often end up enduring extreme long waits in A&E – often on trolleys in corridors.
Figures obtained by RCEM via Freedom of Information Act requests, reveal in England’s major EDs last year, a staggering 1,148,666 people aged 60 and over waited more than 12 hours to be transferred, admitted or discharged.
That’s over 3.5 times more people when compared to 2019, when the figure stood at 305,619.
It also reveals the likelihood of experiencing a 12 hour wait in the ED increases with the age of the patient.
People aged 60-69 have a 15% chance of waiting 12 hours or more, whereas for those aged 90 and above, the likelihood rises to 32.5%.
Against the backdrop of these long waits, RCEM’s research calls on Emergency Department clinicians to recognise and address the distinct healthcare needs and conditions of older adults who are seeking Urgent and Emergency Care.
It also recommends ‘front door frailty screening’ should be in place in every A&E to improve the care they need – something which is being introduced in Scotland.
Dr Adrian Boyle, President of the Royal College of Emergency Medicine said, “The healthcare system is failing our most vulnerable patients – more than a million last year. These people are our parents, grandparents, great-grandparents.
“They aren’t receiving the level of care they need, as they endure the longest stays in our EDs, often Suffering degrading and dehumanising ‘corridor care’.
“It’s an alarming threat to patient safety. We know long stays are dangerous, especially for those who are elderly, and puts people’s lives at risk.
“As our QIP highlights, more needs to be done to improve their care – vital tests need to get underway as soon as they arrive to inform the care they need and mitigate the risk of another visit to the ED.
“There are good pockets of practice, and Emergency Medicine clinicians are trying their best to deliver the care they need. It’s the system that’s the issue and will continue to disproportionally affect older people unless governments across the UK make A&E a political priority.”
Dr Anu Mitra, Project Lead of RCEM’s Care of Older People QIP said: “Older people make up a large proportion of attendances to the Emergency Department, bringing greater health complexities and evolving care needs.
“In the backdrop of worsening crowding and increasing long stays, Emergency clinicians need to ensure they maintain the basic elements of care and comfort for older patients.
“It’s been encouraging to see that despite the challenging environments Emergency Medicine clinicians are working in, there has already been improvements in ensuring these patients are receiving the assessments they need.
“It’s vital we continue this work for this vulnerable patient cohort to meet their needs and provide the level of care they deserve.”
In January this year, the Scottish government announced special ‘frailty teams’ will be placed at the front door of every A&E by summer, to ensure these patients to receive the specialist care and support they need, whether in hospital or back at home.
Meanwhile last year in England, NHSE announced that by April 2025, over 65s will be offered a health ‘MOT’ at the front door to reduce admissions.
