Health Informatics is the internationally recognised and Department of Health term covering the use of resources, devices, and methods required to optimize the acquisition, storage, retrieval, and use of information in health and biomedicine. The number of Emergency Department attendances has been increasing rapidly over the last few years, which has focused attention on why this has occurred.
The Royal College of Emergency Medicine Informatics page features Informatics information and resources including: clinical records, emergency care data set, informatics (and introduction), summary care record and syndromic surveillance. Use the tabs below to browse the resources available.
+ Informatics
Health Informatics is the internationally recognised and Department of Health term covering the use of resources, devices, and methods required to optimize the acquisition, storage, retrieval, and use of information in health and biomedicine.
The number of Emergency Department attendances has been increasing rapidly over the last few years, which has focused attention on why this has occurred.
There are several aspects to the RCEM Informatics group work:
See details of the National Tariff Payment System.
The Professional Record Standards Body (PRSB) has published a Document Naming Standard endorsed by RCEM in May 2019.
The standards for the clinical structure and content of patient records were published in July 2013 by the Academy of Medical Royal Colleges. They were developed through extensive consultation to ensure that they address the requirements of clinicians, patients, carers and health information technology professionals.
Download the standards for the clinical structure and content of patient records.
The Academy of Medical Royal Colleges together with the Royal Pharmaceutical Society (RPS) and Royal College of Nursing (RCN) has produced a report on standards for the design of hospital in-patient prescription charts. The Academy wishes to promote these standards throughout the NHS. The standards were developed by an inter-professional group of doctors, pharmacists and nurses drawn from the medical Royal Colleges, the RPS and the RCN, who reviewed hospital prescription charts from a variety of sources, examined the scientific publications in the area and consulted widely with colleagues in their own organisations and in the NHS using an extensive iterative approach before finalising the recommendations outlined in the report.
See full report and appendices.
The Health and Social Care Act 2012 is the most extensive reorganisation of NHS in England to date. This may act as a powerful stimulus for optimising efficiency and cost effectiveness of care if managed effectively through Clinical Commissioning Groups (CCG). Whilst much of the infrastructure for commissioning is being built, the first 1-2 years will require close co-operation between stakeholders to create and bed down new systems. As witnessed with past events, failure to develop and support an integrated emergency care pathway can potentially result in parts of the pathway becoming overloaded and failing. The commissioning landscape at present can seem confusing to many. Regardless of the new arrangements, Emergency Departments are facing a continuous rise in attendance that shows no indications of declining in an era of reduced financial support, increasing costs of providing 24/7 care and a shortfall in the workforce required to deliver emergency medicine. This page acts as a resource base to support our Fellows and Members with commissioning.
Commissioning the delivery of high quality care in the Integrated Emergency Department – Guidance for Commissioners, clinicians & managers (18 November 2013).
This position paper by the Royal College of Emergency Medicine provides guidance for commissioners, clinicians and managers on how to deliver high quality care in the integrated Emergency Department. This guide recommends ten key recommendations that the College believes should always be considered when the configuration of local EDs are made.
This position statement by the College describes the principles that relevant stakeholders must consider when decisions regarding reconfiguration are being made. These will be especially relevant where stakeholders decide that part of reconfiguration will involve down grading or even closure of an Emergency Department.
Urgent and emergency care: a prescription for the future (18 July 2013) – The Royal College of Physicians, NHS Confederation, the Society of Acute Medicine and the Royal College of Emergency Medicine have set out ten priorities for action to address the challenges faced by urgent and emergency care services. These challenges include:
Download full report: Urgent and emergency care: a prescription for the future
Download the press statement: Press statement from CEM
Mental Health in Emergency Departments – A toolkit for improving care.
Breaking the mould without breaking the system: new ideas and resources for clinical commissioners on the journey towards integrated 24/7 urgent care (1 Dec 2011).
This report has been published by the Primary Care Foundation in partnership with the NHS Alliance. This resource is designed to offer ideas and inspiration to everyone responsible for commissioning urgent and emergency care in the UK, in particular, the new clinical commissioning groups in England.
To provide a more accurate, detailed and complete picture of all emergency attendances, the new Emergency Care Data Set (ECDS) has now launched. The ECDS replaces the Accident and Emergency Commissioning Data Set (CDS type 010).
The good news is Type 1 and 2 Emergency Departments in England are already implementing the mandated changes and submitting new data.
To help staff understand the importance of the ECDS and how they can help support the roll out of this data set, we have developed a simple animation. Please watch our short video and share this with your ED colleagues (including medical, nursing, clerical, reception, operations and management staff).
For more information about the ECDS, please view:
A Summary Care Record stores a defined set of key clinical data for every patient in England who has elected to have one. The majority of the population of England have had an SCR created by their GP practice and uploaded onto the National Spine. As of February 2015 almost 90% of the population, more than 50 million people have a Summary Care Record. SCRs can be accessed electronically by healthcare staff providing care to a patient in an urgent or emergency care setting, anywhere in England, any time of day or night. SCRs provide access to information held on GP clinical systems about, as a minimum, a patient’s medicines, allergies and any past drug reactions. The Summary Care Record is helping to improve safety, and the quality and continuity of care to patients.
Staff viewing a patient’s SCR must be able to demonstrate a legitimate relationship with the patient and must use a smartcard to access the SCR via the secure NHS N3 Network. All accesses will be auditable. The patient’s permission to view must be obtained before the SCR is viewed. If the patient is not able to give properly informed permission to view then a clinical decision can be made to access the record in the patient’s best interest, without first obtaining consent. Such accesses in the patient’s best interest will be recorded and can be investigated should any queries arise about the appropriateness of the access.
SCR viewing can be achieved relatively easily and without incurring significant expense to the provider organisation. A web-based SCR application is available which can provide access to authorised healthcare professionals with a smartcard, via the secure N3 Network, to the Patient Demographic Service (PDS) and to SCRs on the National Spine. Alternatively, embedded information systems which are deployed by some urgent and emergency care providers may provide integrated SCR viewing capability. The same access controls apply. The Summary Care Record Implementation team at the Health and Social Care Information Centre will help organisations that are interested in introducing SCR viewing.
Contact the team at: enquiries@hscic.gov.uk
NHS Digital provides comprehensive implementation advice and up to date information about the benefits of SCR to patients and healthcare staff.
Public Health disease surveillance is the ‘systematic ongoing collection, collation, and analysis of data, and the timely dissemination of information to those who need to know it in order for action to be taken.
In recent years, syndromic surveillance has become an increasingly important tool for disease surveillance. Syndromic surveillance is the collection, analysis, interpretation and dissemination of health-related data, typically on a real-time (or near real-time) basis, to enable the early identification of the impact (or absence of impact) of potential human or veterinary public health threats which require effective public health action.
The EDSSS is a joint project between RCEM and the Health Protection Agency. The data that Emergency Departments routinely collect are anonymised and sent securely to a data warehouse where they are analysed to produce reports. No extra burden is placed on clinicians. Hospitals engaged in this project also have the opportunity to view their own data in real time.
Requests to joint the scheme or for access to data from the project should be sent to the RCEM representatives on the project:
See the HPA website for more information about syndromic surveillance .
The RCEM Informatics committee is performing an audit of the usability of IT systems in Emergency Departments.
The usability (‘user experience’) of IT systems in emergency departments matters to clinicians as these clinical areas have high patient and clinician turnover. This means that training needs and the cost of learning how to operate the IT system is high.
The RCEM informatics committee often hears clinicians complain about their ED IT systems. This is a chance to collect the data that will indicate if usability is a significant issue.
The survey is conducted using a secure app on an Android tablet or phone provided by you. The software will automatically open up and configure itself on the Android device, will be hosted on the same fully secure servers that also holds the RCEM audit data and will be anonymised.
Nothing.
No – the audit is voluntary.
Your system will be rated on a scale of 1-100, most IT systems will rate between 50 and 70. The responses will be collated and then feedback to trusts via the College Informatics Committee.
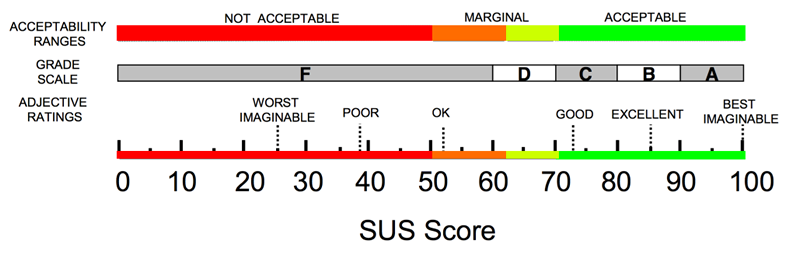
The System Usability Scale (SUS) is a valid and reliable tool for measuring IT usability. It consists of a 10-item questionnaire with five response options for respondents; from ‘strongly agree’ to ‘strongly disagree’.
Originally created in 1986, it allows one to evaluate a wide variety of products and services, including hardware, software, mobile devices, websites and applications.
SUS is the industry standard, with references in over 1300 articles and publications. The benefits of using SUS include that it:
Participants are asked to score 10 items with a response from ‘strongly agree’ to ‘strongly disagree’:
Though the scores are 0-100, these are not percentages and should be considered only in terms of their percentile ranking.
For a computer system with a Graphical User Interface, as with the vast majority of ED IT systems, the mean score is 75, and the standard deviation is 21.
Sample sizes as small as 5 per group have been shown to be surprisingly reliable.
For further information please contact quality@rcem.ac.uk
Aaron Bangor, Philip T. Kortum & James T. Miller (2008) – An Empirical Evaluation of the System Usability Scale, International Journal of Human–Computer Interaction, 24:6, 574-594, DOI: 10.1080/10447310802205776
IT system procurement is usually undertaken at a Trust level and can be bewildering for clinicians involved in the process. We suggest that these issues should be considered during the process. This is clearly not an exhaustive list, and members of the Informatics Committee are happy to help with specific questions.
Some trusts will procure a single electronic record across all clinical areas; others will have a stand-alone ED information system. Where a standalone ED system is procured consideration should be given to how deeply integrated this is with the rest of the trust to minimise switching between systems.
The Health Informatics Unit of the Royal College of Physicians has been pivotal in the development of standards for medical records. It co-ordinated a project that has produced Generic Medical Record Keeping Standards, and Standards for Content and Structure of inpatient notes that have been jointly published by the Academy of Medical Royal Colleges and the NHS Digital and Health Information Policy Directorate.
Hospital admission data are currently available through the Hospital Episode Statistics (HES) database which is a centralised data collection facility covering all NHS and private hospitals in England. Data from this system are available for use for surveillance activities, however the current availability of these data are not timely and are released with an approximate 6 month delay. Therefore, for use in a real-time system HES data are not suitable and more likely to be used for retrospective analyses or validation exercises. There are also costs involved with accessing these data. See more information on hospital episode statistics .
