The RCEM offers grants up to £5,000 for a research application focused on improving the delivery of emergency medicine in low income countries
The RCEM offers grants up to £5,000 for a research application focused on improving the delivery of emergency medicine in low income countries.
The 2025 grant application window is now open
Applications should be submitted by 17:00 BST on May 23rd 2025
Applications should be emailed to policy@rcem.ac.uk
Application form is available here:
Low_Income_Countries_Grant_Application_Form_2025
PLEASE OBSERVE THE WORD AND PAGE LIMITS. APPLICATIONS THAT EXCEED THESE SPECIFICATIONS OR DO NOT HAVE THE RELEVANT SIGNATURES WILL BE DISQUALIFIED. ADDITIONAL MATERIAL MARKED AS ‘SUPPLEMENTARY’ WILL NOT BE REVIEWED.
Applicants must:
For advice on writing a grant application see mrc.ukri.org/
Papers deriving from any successful LMIC grant will be guaranteed external peer review if submitted to the Emergency Medicine Journal – please flag any submissions to Dr Jafar. Leading up to any such submissions, we are working to develop a pool of mentors who can offer writing support in order to give the best possible chance of favourable review.
The following headings should be used:
What is already known in this area and an outline of the value the research will bring to emergency medicine.
Which should include:
Applications are rated according to the quality of science, the importance of the underlying research program, the strength and value of the collaboration with Members and Fellows of the Royal College of Emergency Medicine and contextual relevance. Due regard is given to the relative wealth of the country or countries in which the research will be carried out and the findings acted upon.
Successful applicants are expected to produce a short report in the approved format on the progress of the project every 12 months for the first two years of the award, and may also be invited to present the findings of the study at our Annual Scientific Conference up to three years after the award.
*If no-one in your team is currently a member or fellow of RCEM but you have an interesting/important research idea in emergency medicine, please take a look at colleagues in the NIHR Incubator for Emergency Care who may be able to help support as a co-applicant or link you to further colleagues for this or future submissions
For a list of Frequently Asked Questions (especially important for grant administration information) please see the FAQ section below.
For further information about the grant please contact:
Anisa Jafar,
ST7 in Emergency Medicine on behalf of the Research & Publications Committee.
policy@rcem.ac.uk
+ Do you consider non-emergency care research?
These grants are intended to fund research directly relevant to pre-hospital and facility-based emergency care. All emergency care is part of a continuum and touches upon the range of medical, obstetric, psychiatric and surgical specialities. However we are looking for work which takes place within a country’s emergency care system (or indeed contributes to the development of such a system) i.e. the system whose focus is initial evaluation, diagnosis, treatment, coordination of care for patients with time-critical illness or injury. We often receive high quality proposals which are much more aligned to a speciality and therefore are unlikely to be successful in competition with other good quality proposals with clearer emergency care relevance. If you are in any doubt, please get in touch and we can advise.
Part funding would be considered, especially if there is a natural subsection of the project which could be fully funded. If part funding is granted it will not usually be released until the rest of the funds are obtained, usually with a 6-month time limit.
All applications are rated on the basis of importance to emergency medicine, quality of science, potential for leading to future funded projects, novelty of proposal, potential for research training within the applicant team and feasibility/contextual relevance. Overall value for money will be taken into account as will the clarity of the proposal.
Applications will be discussed in our August committee meetings and funding decisions will be communicated by the end of September. If there is a delay, this may be due to clarification being sought from applicants, and therefore please get in touch only if you have not had communication by the end of September.
Pilot studies that have the potential to lead to a Grant Application to another major funders of emergency medical research will be considered.
Worthwhile sub-studies can be considered.
In these circumstances it is unlikely that your application will be successful, unless a very good argument can be made about why the initial funding has not been sufficient.
Generally surveys are less robust in terms of research methodology and would be unlikely to be funded unless they had appropriate justification.
We would not automatically reject a quality improvement study however it would very much depend how strong it was in its own right and also in comparison to other submissions in the grant round because the primary intention of this grant was not aimed at QI.
In general we do not fund the setting up of registries as the sole purpose of the research grants. If it could be demonstrated to be an integral part of the broader question and there was a defined plan to use the funding to answer a research question, it might be considered.
Secondary research may be supported however justification of funding would need to be very clear.
Using the latest DAC List of ODA Recipients our primary aim is to fund research in the Least Developed Country (LDC), Low Income Country (LIC) and Lower Middle Income Country (LMIC) categories. Upper Middle Income Countries (UMICs) are not precluded from applying, particularly those whose healthcare systems have been challenged by natural or man-made disasters or who are strongly projected to drop into the LMIC category. However, it is at the discretion of the panel to balance whether the application, in comparison to other submissions from LDC/LIC/LMICs, makes the case for addressing a specific need in developing emergency care.
All proposals should stick within the page/word count as indicated on the application form or they risk rejection: we cannot guarantee screening of submissions and request for re-submission in the same grant round, so the responsibility lies with the lead applicant. If there is no co-applicant who is a member or fellow of RCEM then the application will not be accepted.
If a previous awardee has failed to demonstrate satisfactory progress and engagement via their annual reports, then they would be considered ineligible.
Our funds are limited and we seek to fund as widely as we possibly can. Therefore we would not make two awards in any one year to the same lead applicant. Whilst we would not rule out giving more than one award to the same institution, we would expect that the topics of the proposal to be very different and if there were two equally competing applications for a second award, it is highly likely we would award to the different institute to broaden our impact as a funder.
If you are not successful you may re-apply in other grant rounds, clearly indicating this is a resubmission, however if you receive feedback and do not act upon it, we reserve the right to automatically reject the proposal without review (as time will have already been spent reviewing and making suggestions). It is possible that an application is deemed unfundable but the panel believe there is potential for revision and re-submission within the same round, in which case this will be fed back and a hard deadline for revision will be given (usually in the region of 4-6 weeks). If the deadline is not met and/or the areas of concern are not addressed sufficiently then the revision will almost certainly be rejected at that point except in very exceptional circumstances (any extensions request to deadlines would need to be very clearly justified). Further resubmission in later grant rounds would usually be permitted however feedback would very clearly need to have been taken on board.
We encourage all applicants where possible to list a local academic institution who will administer the grant funds. Alternatively the local hospital employing the applicant can perform the same role. If this is not possible, a recognised national emergency medicine society may be able to support in this role.
The use of an NGO to administer the funds should be avoided, but if deemed absolutely necessary will require RCEM to undertake due diligence and cannot be guaranteed to be approved pending the outcome. We discourage applicants to apply without an administering organisation because this will require the applicant to spend out of pocket and the process of claiming back funds can create significant delay.
It should be noted that any organisation taking on the role of administration can be costed to a maximum of 10% of the total grant. In 2023, this 10% would need to be encompassed within the £5000 total grant budget. We are in discussion for future years as to whether we can accommodate the 10% beyond the £5000 total.
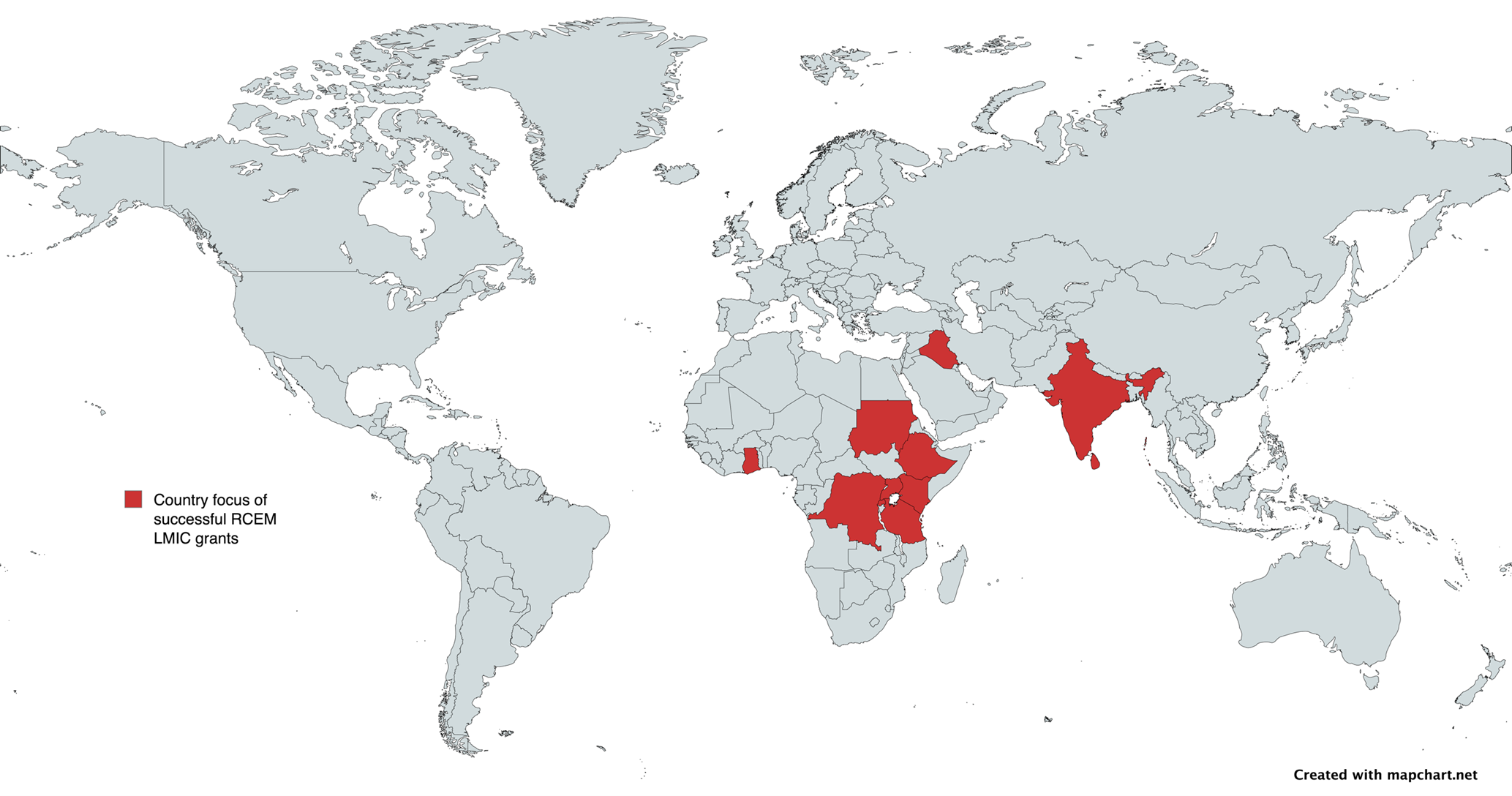
| Year | Study Title | Funds Awarded | Principal Investigator |
|---|---|---|---|
| 2024 | Diagnostic Accuracy of Lung Ultrasound for Pulmonary Tuberculosis Among HIV Positive Adult Patients in a Low-resource Setting. | £5,000 | Dr Kwagala Racheal |
| 2024 | Improving recognition and treatment of deteriorating patients in Kilifi County Referral Hospital | £4,968 | Dr Jasdeep Bahra |
| 2022 | Prevalence, associated factors and interventions of burnout & work-place stress in ED health workers & trainees in Uganda | £4,173 | Dr Jonathan Kajjimu |
| 2021 | The application of mobile software to decrease length of stay in the Emergency Medicine and critical Care department of Hiwot Fana specialized university hospital, Harar, Ethiopia | £1,859 | Asst. Professor Nathan Muluberhan |
| 2021 | Paediatric trauma tele-simulation training: A novel solution to sustainable affordable emergency care capacity building in India | £4,750 | Dr Ankur Verma |
| 2020 | An exploration of factors that influence the implementation and establishment of formal triage systems in Uganda | £5,268 | Dr Najeeb Rahman |
| 2020 | Sri Lanka Out-of-Hospital Cardiac Arrest Study (SLOCAS) | £5,000 | Dr Kaushila Thilakasiri |
| 2020 | Trauma Assessment, Procedures and Pathways in the Emergency Department (TrAPPED): A Rwandan Study | £5,000 | Dr Najeeb Rahman |
| 2019 | The development of a community first aid responder programme in the Democratic Republic of Congo | £5,000 | Dr Ken Ngoy Diango |
| 2018 | Reform of emergency care in low-income countries | £5,000 | Dr Ahmed Eltahir Osman Ali |
| 2016 | Estimating the weight of children and adults in emergency medicine | £1,381 | Appolinaire Manirafasha |
| 2016 | Strengthening Emergency Care Systems in Low Income Countries | £6,259 | Lee Wallis |
| 2016 | Senior Doctor Initial Assessment in Triage: Staff Perspectives | £6,230 | Zakaria Marwarn |
+ Diagnostic Accuracy of Lung Ultrasound for Pulmonary Tuberculosis Among HIV Positive Adult Patients in a Low-resource Setting.
Improving recognition and treatment of deteriorating patients in Kilifi County Referral Hospital
Date of award: September 2024
Lead applicant: Dr. Jasdeep Bahra jasdeep.bahra@gmail.com
Type of research: Implementation study
Country(ies) involved: Kenya
HIC partner: Dr. Alex Novak, Director of Emergency Medicine Research Oxford (EMROx), alex.novak@ouh.nhs.uk
Summary of project:
Future Health Africa’s Global Recognition of the Acutely Sick patient and Initial Treatment (GRASPIT) course and the National Early Warning Score (NEWS2) two interventions widely shown to improve emergency care outcomes, however there is a lack of evidence to support their use in Low-Middle income countries. Kilifi County Referral Hospital (KCRH) is on the Kenyan Coast currently lacking emergency care training and standardised patient observation recording leading to delayed patient escalation.
This study aims to introduce GRASPIT & NEWS2 charts into KCRH and assess their impact on mortality, accurate recording of patient observations & correct escalation procedure.
Publications/presentations: not yet commenced
Diagnostic Accuracy of Lung Ultrasound for Pulmonary Tuberculosis Among HIV Positive Adult Patients in a Low-resource Setting.
Date of award: August 2024
Lead applicant: Dr Kwagala Racheal kwagala.racheal@yahoo.com
Type of research: Cross-sectional study
Country(ies) involved: Uganda
HIC partner: A/Prof. Adjunct Mary Ellen Lyon, Yale University maryellen.lyon@yale.edu
Summary of project:
Diagnosing TB in resource-limited settings is challenging due to limited access to diagnostic tests, posing barriers to timely treatment initiation. The WHO’s “End TB Strategy” emphasizes the need for improved diagnostic methods. Lung Ultrasonography (LUS) is emerging as a promising inexpensive, fast, portable, and non-irradiating alternative. LUS’ performance in pneumonia diagnosis is well studied, however, its role in TB diagnosis is under-researched. This study aims to determine the sensitivity and specificity of LUS, by a resident in emergency medicine, for pulmonary TB (PTB) diagnosis by comparing LUS findings to sputum Gene Xpert results as a reference standard.
Publications/presentations: not yet commenced
Date of award: October 2023
Lead applicant: Dr.Janet Jebichii Sugut dr.janetsugut@gmail.com
Type of research: Observational study
Country involved: Tanzania
HIC partner: Prof Ellen Weber, University of California San Francisco Weber, ellen.weber@ucsf.edu
Summary of project:
Many emergency departments do not routinely perform basic screening for blunt cardiac injury (BCI). Therefore the incidence and outcome of BCI in low-middle income countries is not known, making it unclear whether scare resource should be used to screen for it. Furthermore, the follow-up pathways for any positive-screened patients is unclear.
This prospective observational cohort study seeks to establish the incidence, predictors and 7-day outcomes of BCI among blunt chest trauma patients attending ED of Muhimbili National Hospital.
Publications/presentations: project complete
Poster presentation: 12th MUHAS Conference June 27th-28th, 2024 held at the East African Center of Excellence for Cardiovascular Health, Mloganzila-Dar es Salaam, Tanzania.
End of Life Care Decision Making and Communication in the Emergency Department: A Mixed Methods Study.
Date of award: September 2023
Lead applicant: Dr. Anita Eseenam Agbeko aeagbeko@gmail.com
Type of research: Mixed methods
Country(ies) involved: Ghana
Summary of project:
To feed into the development of emergency department (ED)-specific end-of-life (EoL) care decision-making and communication models, this study proposes to ascertain how ED practitioners communicate and make EoL decisions. It uses a cross-sectional approach to collect data using 3 validated tools from ED practitioners at the Komfo Anokye Teaching Hospital. This is followed by face-to-face interviews exploring in-depth how they navigate through EoL decision-making and communication.
Publications/presentations: Data collection/analysis in progress
Prevalence, associated factors and interventions of burnout & work-place stress in ED healthworkers & trainees in Uganda
Date of award: August 2022
Lead applicant: Dr Jonathan Kajjimu (jonathkebenz37@gmail.com)
Type of research: Mixed methods study
Country(ies) involved: Uganda
HIC partner: A/Prof. Shweta Gidwani, Chelsea & Westminster ED – shwetagidwani@gmail.com
Summary of project:
Using a descriptive cross-sectional survey, in-depth interviews and focus group discussions to study the extent of the threat of burnout, contributing factors and potential solutions amongst healthcare workers in Ugandan emergency departments Ugandan with a view to advocating for appropriate resources to support staff retention.
Publications/presentations: Data analysis projected for September 2024
RCEM ASC Gateshead 2024 (LMIC grant update session)
Using tele-simulation to build capacity for paediatric emergency medicine trauma care in health care workers in India
Date of award: December 2021
Lead applicant: Dr Ankur Verma anksv25@gmail.com
Type of research: Mixed methods study
Country(ies) involved: India
HIC partner: A/Prof. Shweta Gidwani, Chelsea & Westminster ED – shwetagidwani@gmail.com
Summary of project:
Using India as a case example, we will create contextually appropriate paediatric trauma cases and develop detailed case scenarios which we will then use to create moulage videos. The knowledge and competency levels will be set for a variety of different health care providers and the content will be based on established standards of care such as the WHO BEC course and ATLS principles. We will then test the content material with trainers and finally deliver the paediatric trauma tele-simulation training to a variety of different health care providers based on the existing learning from tele-sim. Through, surveys, focus group discussions and interviews of the participants we will assess the value of this intervention while also exploring the challenges.
Publications/presentations: project complete
Abstract in IFEM Trauma Special Interest Group August 2024 newsletter
RCEM ASC Glasgow 2023 (LMIC grant update session)

The application of mobile software to decrease length of stay in the Emergency Medicine and critical Care department of Hiwot Fana specialized university hospital, Harar, Ethiopia: Quasi-Experimental study design
Date of award: December 2021
Lead applicant: A/Prof. Nathan Muluberhan natanxy@gmail.com
Type of research: Quasi-experimental/quality improvement
Country(ies) involved: Ethiopia
HIC partner: Prof Ellen Weber, University of California San Francisco Weber, ellen.weber@ucsf.edu
Summary of project:
The project aims to calculate the length of stay for patients admitted to the Emergency department of Hiwot Fana specialized university hospital, Harar, Ethiopia. It then aims to identify the factors influencing prolonged length of stay using survey data and focus groups. Subsequently, after implementing a mobile phone notification system (developed during the study) which will provide real-time data to staff regarding length of stay and those likely to have prolonged stays, the research team will calculate whether there has been a decrease in length of stay for patients overall.
Publications/presentations:
Submitted paper to African Journal of Emergency Medicine
RCEM ASC Gateshead 2024 (LMIC grant update session)
Trauma Assessment, Procedures and Pathways in the Emergency Department (TrAPPED): A Rwandan Study
Date of award: December 2020
Lead applicant: Dr Najeeb Rahman najeebrahman@nhs.net
Type of research: Mixed methods study
Country(ies) involved: Rwanda
HIC partner: Dr Najeeb Rahman, Leeds Teaching Hospitals NHS Trust ED – najeebrahman@nhs.net
Summary of project:
Trauma represents a significant burden in Rwanda, accounting for more than 50% of emergency department admissions to the primary referral hospital in Kigali. However, there is little published literature on the details of trauma pathways. This study sought to describe the features and characteristics of current trauma care for adults at 2 national referral hospital sites in Kigali, thereby contributing to pathway description and recommendations for improvement.
Publications/presentations: data collection complete, write-up in progress
RCEM ASC Glasgow 2023 (LMIC grant update session)
Sri Lanka Out-of-Hospital Cardiac Arrest Study (SLOCAS)
Date of award: November 2020
Lead applicant: Dr Kaushila Thilakasiri kaushila@gmail.com
Type of research: Observational study
Country(ies) involved: Sri Lanka
HIC partner: Prof. Andrew Lockey, Calderdale & Huddersfield ED – andrew.lockey@resus.org.uk
Summary of project:
The purpose of this observational research is to analyse data associated with out-of-hospital cardiac arrest (OHCA) in Sri Lanka, using the existing platform of “Suwaseriya”: the free national ambulance Service. This will help to estimate the scale of the problem of OHCA in Sri Lanka for the first time. This research will be valuable in developing policies and strategies to implement both by-stander CPR training and public-access automated external defibrillators along with expansion of emergency ambulance services to reduce preventable deaths in developing countries.
Publications/presentations: data collection in progress since Sept 2023
Related work:
Thilakasiri K, Wijegunawardana PK, de Silva S, Fernando S, De Silva SL. “1990 Suwa Seriya” the national pre-hospital care ambulance service of Sri Lanka; a narrative review describing the EMS system with special emphasis on Out of Hospital Cardiac Arrest (OHCA) in Sri Lanka. Resuscitation Plus. 2024 Sep 1;19:100649.
RCEM ASC Glasgow 2023 (LMIC grant update session)
An exploration of factors that influence the implementation and establishment of formal triage systems in Uganda
Date of award: January 2020
Lead applicant: Afizi Kibuuka najeebrahman@nhs.net
Type of research: Mixed methods study
Country(ies) involved: Uganda
HIC partner: Dr Najeeb Rahman, Leeds Teaching Hospitals NHS Trust ED – najeebrahman@nhs.net
Summary of project:
Early recognition of serious illness and injury is critical to reducing mortality and morbidity and is a pillar of emergency care. The Triage Interventions, Processes and Procedures in the Emergency Department (TrIPPED) study sought to explore the factors that influence implementation and establishment of the formal triage systems in Uganda. This was done by conducting staff surveys, interviews as well as observation in 4 referral hospitals in Uganda. The project was primarily managed by local Ugandan colleagues. One of the key objectives was to ensure commentary from a ‘human factors’ perspective so as to pragmatically inform stakeholders on triage establishment.
Publications/presentations:
RCEM ASC Virtual 2021
The development of a community first aid responder programme in the Democratic Republic of Congo
Date of award: November 2019
Lead applicant: Dr Ken Ngoy Diango k.d.ngoy@gmail.com
Type of research: Mixed methods study
Country(ies) involved: Democratic Republic of Congo
Summary of project:
This project aim is to develop a country-specific Community First Aid Responder (CFAR) programme as an initial step to increasing prehospital capacity.
The first part of the study is a baseline evaluation which mapped the DRC emergency care system using the WHO Emergency Care System Assessment tool
The second part is a community-based cross-sectional survey which evaluated the needs and supply of emergency care in Kinshasa, DRC. Concomitant to this survey, the research team evaluated the awareness, attitude and perceived knowledge regarding First Aid in Kinshasa’s households.
The third part on needs assessment and acceptability of a CFAR programme in Kinshasa, DRC is a qualitative study
The last part on the implementation and evaluation of a pilot World Health Organisation’s Community First Aid Responder training in Kinshasa, DRC is a mixed methods analysis delving into a methodical evaluation of key aspects of the implementation of a pilot CFAR training and perspectives of both organisers and participants in order to inform future rollouts and related research.
Publications/presentations:
DRC Emergency Care System Assessment Report.
Diango K, Yangongo J, Sistenich V, et al. Evaluation of needs and supply of emergency care in Kinshasa, Democratic Republic of Congo: a cross-sectional household survey. BMJ Open 2022;12:e060036. http://dx.doi.org/10.1136/bmjopen-2021-060036
Diango K, Yangongo J, Sistenich V, et al. Awareness, attitude and perceived knowledge regarding First Aid in Kinshasa, Democratic Republic of Congo: A cross-sectional household survey. https://doi.org/10.1016/j.afjem.2022.03.001
Reform of emergency care in low-income countries
Date of award: January 2018
Lead applicant: Dr Ahmed El tahir Osman Ali ahmedaltahir@gmail.com
Type of research: Operational health system research
Country(ies) involved: Sudan
HIC partner: Prof. Richard Body, Manchester Royal Infirmary ED – richard.body@manchester.ac.uk
Summary of project:
LMIC emergency care system reform data will be scoped using a systematic review of the literature. This will be followed by an assessment of 10 emergency units in Sudan using the WHO Emergency Unit Assessment Tool to generate baseline data.
6-months of process and clinical outcome (mortality) data will be collected from the each unit on 5 sentinel conditions (paediatric diarrhoea, pneumonia, asthma, road crashes, post-partum haemorrhage) as a baseline from which to measure impact. Sn individualised, site-specific improvement plan will then be driven by the results of the assessment and implemented in an initial concentrated package, followed by ongoing training and support
Publications/presentations: Political instability in Sudan led to the re-focussing of this grant which will now study a qualitative evaluation of emergency care system interventions with a focus on the Interagency Integrated Triage Tool (IITT) and WHO clinical checklists in low and middle-income countries (LMIC). The expected outputs are envisaged to provide a better understanding of how to incorporate qualitative elements into designing and evaluating emergency care system interventions.
Senior Doctor Initial Assessment in Triage: Staff Perspectives
Date of award: August 2016
Lead applicant: Zakaria Marwarn Mariozakaria00@gmail.com
Type of research: Qualitative study
Country(ies) involved: Iraq
Summary of project: A qualitative study exploring the perspectives of emergency doctors on the implementation of triage, their experience, and the effect on patient care in Iraqi hospitals.
HIC partner: Prof. Suzanne Mason, University of Sheffield – s.mason@sheffield.ac.uk
Strengthening Emergency Care Systems in Low Income Countries
Date of award: August 2016
Lead applicant: Lee Wallis lee.a.wallis@gmail.com
Type of research: Epidemiology
Country(ies) involved: Tanzania & Uganda
Summary of project: Mortality and process data were collected on 6000 patients over 12 months at 4 district hospitals – 2 in Tanzania, 2 in Uganda – who presented at the emergency unit with 1 of 5 sentinel conditions: injury, pneumonia, asthma, paediatric gastro, or post-partum haemorrhage. Overall mortality rate was 3.27% across all sites.
Beyond the grant, the next phase of the project involves the implementation of an emergency care intervention package developed by WHO. Post-intervention data have been collected immediately after implementation at each site and a comparative analysis of pre- and post- intervention data will be performed to evaluate the impact of the intervention. A post intervention sample of 6000 patients has been recruited.
Publications/presentations: the work informed WHO’s evidence base for impact of emergency care interventions but has not yet been published in the scientific literature.
Estimating the weight of children and adults in emergency medicine & accuracy of weight estimation methods in adults, adolescents and children: a prospective study
Date of award: August 2016
Lead applicant: Appolinaire Manirafasha maniappo@gmail.com
Type of research: Derivation/validation study
Country(ies) involved: Rwanda
HIC partner: Dr Giles Cattermole, Kings College Hospital ED – giles@cattermole.org.uk
Summary of project:
First study question compared the accuracy of various weight estimation methods to derive a dedicated age-based tool within a Rwandan setting.
Second study question assessed weight estimation methods in patients of all ages in Rwanda compared to other methods used in developed countries
Publications/presentations
RECA Kigali 2017 (oral presentation & abstract published in AfJEM)
RCEM ASC Liverpool 2017 (poster presentation x2)
RCEM Research Engagement Day Virtual 2022 (oral presentation)
Manirafasha A, Yi S, Cattermole GN. Estimating children’s weight in a Rwandan emergency centre. African J Emerg Med 2018; 8: 55–58
Cattermole GN, Manirafasha A. Accuracy of weight estimation methods in adults, adolescents and children: a prospective study. Emerg Med J 2021; 38: 718-723