The Committee has a clear remit to:
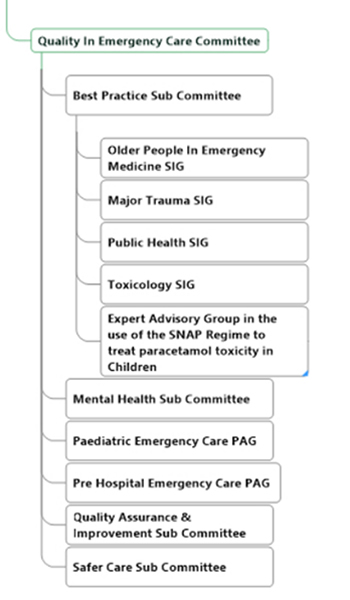
The Quality in Emergency Care Committee (QECC) is part of the RCEM Quality Cluster. A small steering group of Sub-Committee Chairs meets twice a year and there are two large committee meetings each year for all QECC members. The committee is currently chaired by James France. The Quality in Emergency Care Committee consists of a number of diverse Sub-Committees, Special Interest Groups (SIGs) and Professional Advisory Groups (PAGs), as shown below.
The current QECC Chair is James France.
+ Best Practice Subcommittee
The Best Practice Sub-Committee (BPC) produces guidelines where clinical evidence is limited, but where there is a perceived clinical need by members / fellows. This work is almost unique amongst medical royal colleges. The Best Practice Sub-committee also oversees the work of the following Specialist interest groups (SIGs).
Provides advice and guidance on issues relating to older persons attending the emergency department (ED). SIG activity includes holding study days.
Provides advice and guidance related to public health and health inclusion relevant to the emergency department. SIG activity includes holding study days.
Provides advice and guidance on issues related to the treatment and assessment of patients attending the emergency department following exposure to toxic substances. The SIG is responsible for liaising with the National Poisons Information Service regarding the antidotes (specific treatments for exposure to toxic substances) that should be held by each emergency department in the UK. SIG activity includes holding study days.
The current Best Practice Chair is Paul Hunt
To be confirmed.
For further information please contact Quality@rcem.ac.uk
The Quality Audit & Improvement sub-committee is responsible for overseeing the Quality Improvement Projects which are offered to every emergency department in the UK. These quality improvement projects take a specific aspect of emergency department care and aim to improve the quality of care for patients with this condition; the projects run over a period of one to three years. The work of the sub-committee includes advice on the procurement of the computer platform required to run the national audit programme as well as clinical standard setting and the production of national reports.
The current Co-chairs of QI&A are Fiona Burton & Dale Kirkwood
To be confirmed.
To be confirmed.
For further information please contact Quality@rcem.ac.uk
The Mental Health Sub Committee role is to produce advice on how to look after patients in Mental Health Crisis. Keeping these patients safe and ensure they are treated with respect and dignity. We work closely with the other Royal Colleges, services such as the Police, Paramedics and Social Care to try and improve access to support with in the emergency department and the community.
The current Mental Health Chair is Mark Buchanan
To be confirmed.
To be confirmed.
RCEM has an active Mental Health Committee whose role is to produce guidelines and resources to equip RCEM members and fellows, with the aim of improving care, safety and patient experience for patients with mental health problems. We also do advocacy and liaison work with other National bodies including other royal colleges, the college of policing, and the CQC.
RCEM learning. There are some great podcasts and learning modules.
Mental Health services for children and young people (CYP) in crisis in the Emergency Department (ED) have long been a concern for staff, patients, and carers. Children, young people, and their carers often have few alternatives than to come to the ED when in crisis, even those already being cared for by CAMH services. RCEM conducted a survey of availability of services for this group of patients in UK Emergency departments in 2018, and repeated it in 2020 to assess progress since then. Bother surveys can be found below.
Previous updates to mental health leads about what is happening in Emergency Mental Health Nationally and at RCEM.
This quiz will take you 2-3 minutes, just to get you thinking.
Do you have a system for mental health triage in your ED?
This is the probably the most important intervention to improve safety for mental health patients. Who trains your nurses to do this? (Hopefully your liaison team are fully engaged with this!) See toolkit for ideas.
Do you have a process for observing those patients that you are most concerned about leaving the ED or self-harming?
Often health care assistants take this role, do you ever speak to them about patients to ask what they have observed? Can you work together to help the patient feel safe and well cared for? HCAs often report not knowing what to say or look for with some patients. Do you have any resources for patients to reduce anxiety? E.g. mindfulness exercises, colouring, soduku, etc?
Do you know your local 24/7 mental health crisis phone number (most introduced since Covid) to give to patients that may need help?
NHS urgent mental health helpline (England only)
Can you name any or all of the Liaison Psychiatry / Crisis team nurses and doctors that see patients in your department?
Try a charm offensive, get to know them, learn from them, get feedback from them.
Are you ever aware of poor staff attitudes towards patients with mental health problems who attend frequently?
Could you challenge these attitudes and be the patient’s advocate?
Have you ever had these attitudes yourself?
Ask yourself why? Were you tired? Annoyed at the system? or perhaps not had / taken the time to find out why this patient landed in the ED and how they feel?
If you think you could be an advocate for better services and care in your department, why not contact (or become?!) your ED mental health lead.
The Royal College of Emergency Medicine recently launched the RCEM Wellbeing App to provide Fellows and Members with the tools they need to measure, understand and improve their mental wellbeing. It can be found here.
For queries or more information email mhchair@rcem.ac.uk
For further information please contact Quality@rcem.ac.uk
The safer care sub-committee provides advice and guidance on issues relating to patient safety within emergency departments. The sub-committee works closely with other NHS bodies as well agencies such as the Healthcare Services Safety Investigation Body (HSSIB). The sub-committee produces regular safety bulletins as well as holding study days.
The current Safer Care Sub-committee Chair is Dr Emma Redfern.
To be confirmed.
To be confirmed.
For further information please contact Quality@rcem.ac.uk
Provides advice and guidance on issues relating to older persons attending the emergency department (ED). SIG activity includes holding study days.
The current OPEM Chair is Rachel Morris
To be confirmed.
Welcome to the webpage of the Special Interest Group (SIG) for older people at the Royal College of Emergency Medicine.
We are very interested to hear from you about projects and ideas you may have to improve the care of older people in our emergency departments.
Older people are increasingly important attendees to UK’s emergency departments. They are a heterogeneous group and many are active and well although a small proportion are frail.
The fact that older people comprise a special group of ED attendees was described some time ago and many of the conclusions are ever more important.
The report from QualityWatch described the complexity in presentation associated with age and its impact on ED attendances.
RCEM was instrumental in supporting the Silver Book project and this SIG is a concerted effort to bring together like-minded people keen on improving quality care for older people in UK EDs through leadership, service improvement, research and education.
Here are links to some websites on Geriatric Emergency Medicine from around the world that demonstrate the excellent work being undertaken on improving older peoples care.
For further information please contact Quality@rcem.ac.uk
Provides advice and guidance related to public health and health inclusion relevant to the emergency department. SIG activity includes holding study days.
The current Public Health Chair is Fedel Frederico
To be confirmed.
We all recognise how the Coronavirus pandemic has exposed health inequalities and how more so now than ever the relevance of public health and the role we play as emergency physicians in improving the nation’s health, as well as our response to infectious disease control in the emergency department and the wider urgent and emergency care system.
Public health underpins everything we do, even if you do not know it. For example, do you ever get frustrated by seeing the same sort of preventable injuries and illnesses coming through the front door of your Emergency Department (ED)? What about the injured child cyclist? The adult with recurrent alcohol, tobacco, or drug-related illness? Presentations due to failures in under-resourced community and social care systems? People struggling with mental health problems because they have nowhere else to turn? Social deprivation, alcohol, drugs and adverse mental health are inextricably linked and widen health inequalities with higher levels of preventable illness such as injury related to road traffic accidents, cardiovascular disease and infectious disease with lower socioeconomic status. The ED has annual patient-doctor interactions in the tens of millions, but how often do we take the opportunity to think about the “bigger picture”, let alone have a positive impact on it?
The RCEM Public Health Special Interest Group was established in January 2017 with the vision to provide an integrated approach to strengthening the interface between public health and emergency care in order to improve health outcomes for communities. We are currently made up of 6 clinicians and 1 lay member (names below) who hope to achieve this vision through:
As a Special Interest Group, we have developed partnerships with key stakeholders and been active in education and curriculum development, research and policy and media engagement. Our initial priority area was injury prevention. Our priority for the next three years is health inequalities and preventative approaches in emergency departments. For trainees this is a particularly exciting time as public health is incorporated into the 2021 emergency medicine curriculum and we plan to support you with resources.
Below is a summary of our work in these areas and future plans.
The following resource has been released by NHS England highlighting 8 urgent points that need to be addressed in order to tackle health inequalities.
The Kings Fund summarises what are health inequalities, inequalities in life expectancy, healthy life expectancy, avoidable mortality, long-term conditions, mental ill-health, access and experience of health services, plus pathways to health inequalities, interactions between the factors driving health inequalities.
The Kings Fund regularly update their health inequalities page with topical and interesting articles.
Further health inequalities resources can be found on the Health Foundation Page
The NHS Long Term plan outlined aims and objectives for the NHS over a ten year period. Chapter 2 involved new funded action the NHS will take to strengthen its contribution to prevention and health inequalities.
The Health Foundation commissioned the Institute of Health Equity to examine progress in addressing health inequalities in the UK, 10 years on from the landmark study Fair Society, Healthy Lives (The Marmot Review). The following resource explores the changes since 2010 in 5 key objectives, outlining areas of progress and decline of each as well as recommendations for future actions.
Research showing the association between the current pandemic and health inequalities has been definitive. The following links highlight just a small selection of key resources describing this association.
The following videos are a great resource for preventing vaccine hesitancy within ethnic minorities:
Upcoming events
You can email the Public Health chair: PHChair@rcem.ac.uk, Public Health administrator quality@rcem.ac.uk, or tweet us at @RCollEM and use#RCEMPH.
The group have set up a WhatsApp group to coordinate engagement with public health and emergency medicine colleagues.
Fedel Federico (chair), Dr Kirsty Challen, Dr Najeeb Rahman, Mr Martin Rolph (Lay), Dr Thomas Shanahan, Dr Andy Snell and Dr Olivia Villegas
Help for doctors with more severe current anxiety or depression symptoms now.
BMA – 24/7 counselling service (0330 123 1245)
BMA – counselling and peer support
Papyrus – Hopeline
RCEM has put together 2 posters to display in our staff areas with advice about individual and team (herd) wellbeing:
For further information please contact Quality@rcem.ac.uk
Provides advice and guidance on issues related to the treatment and assessment of patients attending the emergency department following exposure to toxic substances. The SIG is responsible for liaising with the National Poisons Information Service regarding the antidotes (specific treatments for exposure to toxic substances) that should be held by each emergency department in the UK. SIG activity includes holding study days.
The current Public Health Chair is Rizwan Riyaz
Tbc – chair
For further information please contact Quality@rcem.ac.uk
The EPRR PAG provides expert advice to the College on matters relating to major incidents; CBRNE (Chemical, Biological, Radiological, Nuclear, and high yield Explosives) incidents and other EPRR specialist incidents. It liaises with various national bodies including NHS England, NARU and UKHSE.
The current chair of EPRR PAG is to be confirmed.
To be confirmed.
Details to follow.
For further information please contact Quality@rcem.ac.uk
The group has a wide remit with representation from other paediatric interest groups, committees and colleges. Its objective is to assist the college with its position on issues relating to paediatric emergency medicine. It also aims to provide practical advice and guidance to members and fellows of the college. The group also collaborates with other groups both within and external to the college on projects relating to paediatric emergency medicine.
The current chair of PEM PAG is Rob Stafford.
To be confirmed.
Details to follow.
For further information please contact Quality@rcem.ac.uk
Prehospital Emergency Medicine (PHEM) is a GMC recognised subspecialty of Emergency Medicine and a number of RCEM Members and Fellows work in the prehospital setting on air ambulances, as first responders, or in community emergency medicine schemes. The Professional Advisory Group provide advice on issues relating to the prehospital care of patients before they arrive at the Emergency Department. This includes collaborating with other prehospital organisations, developing guidelines and quality improvements, supporting career advice for PHEM and holding educational study days.
The current chair of PEM PAG is Caroline Leech
To be confirmed.
Details to follow.
For further information please contact Quality@rcem.ac.uk
