Our emergency departments are under ever increasing pressure, with performance in winter reaching new lows every year; putting both patient safety and staff morale at risk.
While a significant increase in resources, for both the NHS and social care, is clearly needed there are actions that health service leaders and boards can take to help their systems maintain safety and improve performance over winter.
Here we outline those actions and call on health service leaders to encourage whole system ownership of ED performance, with every part of the hospital understanding the importance.
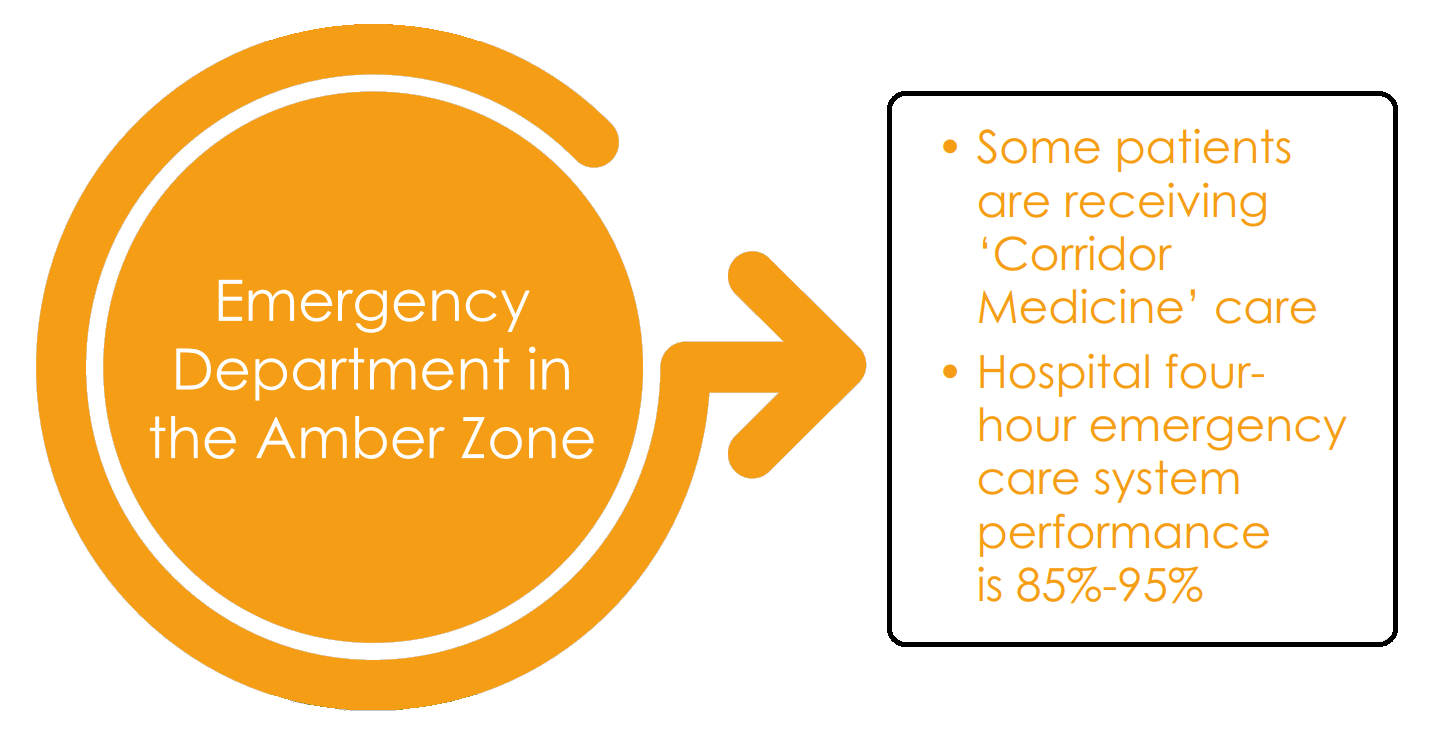
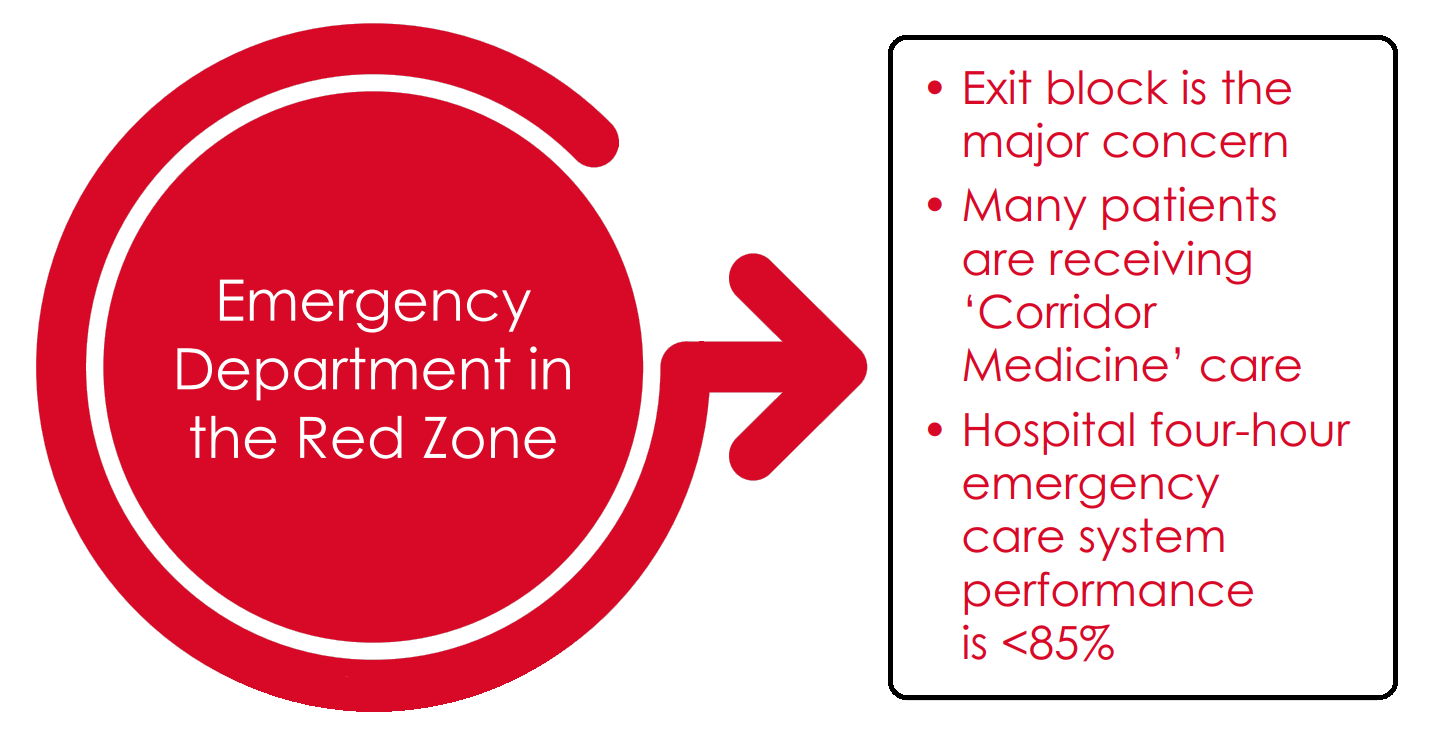
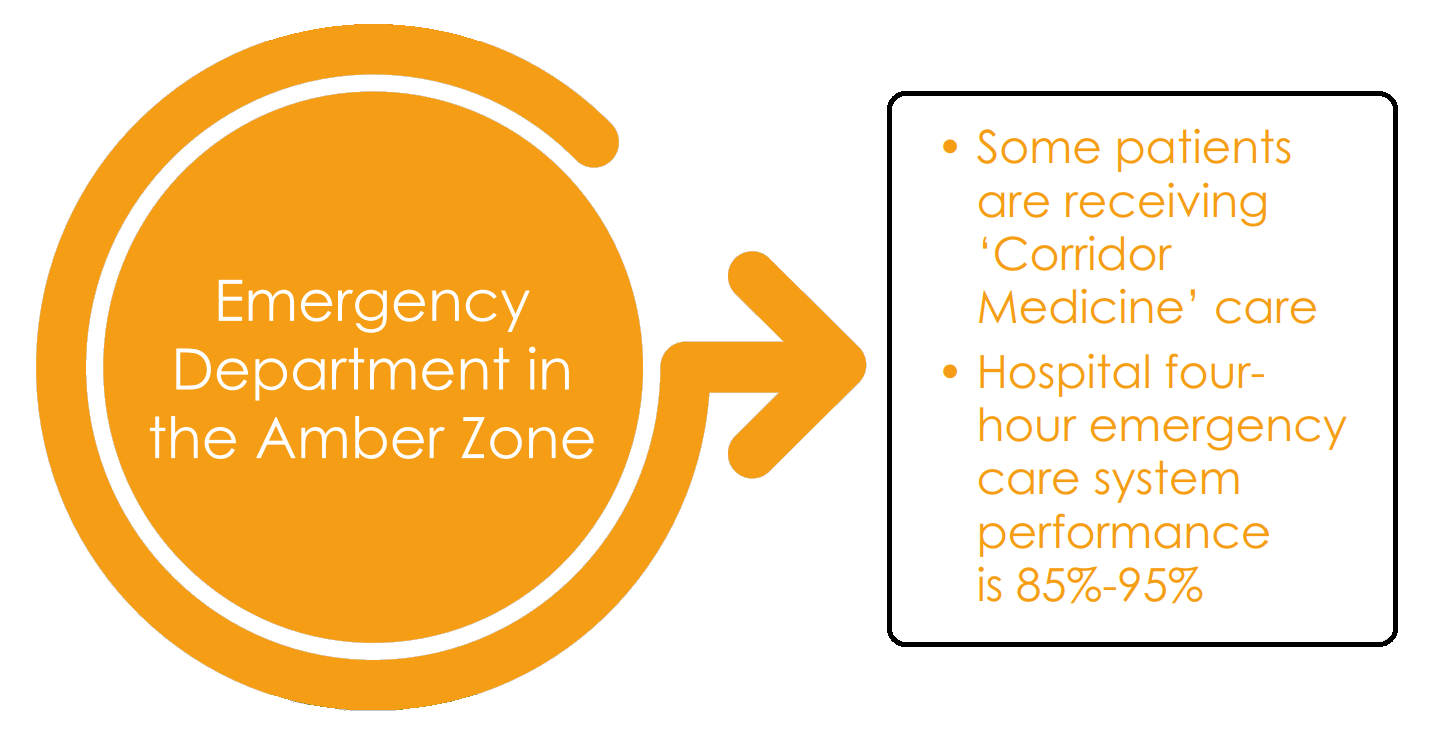
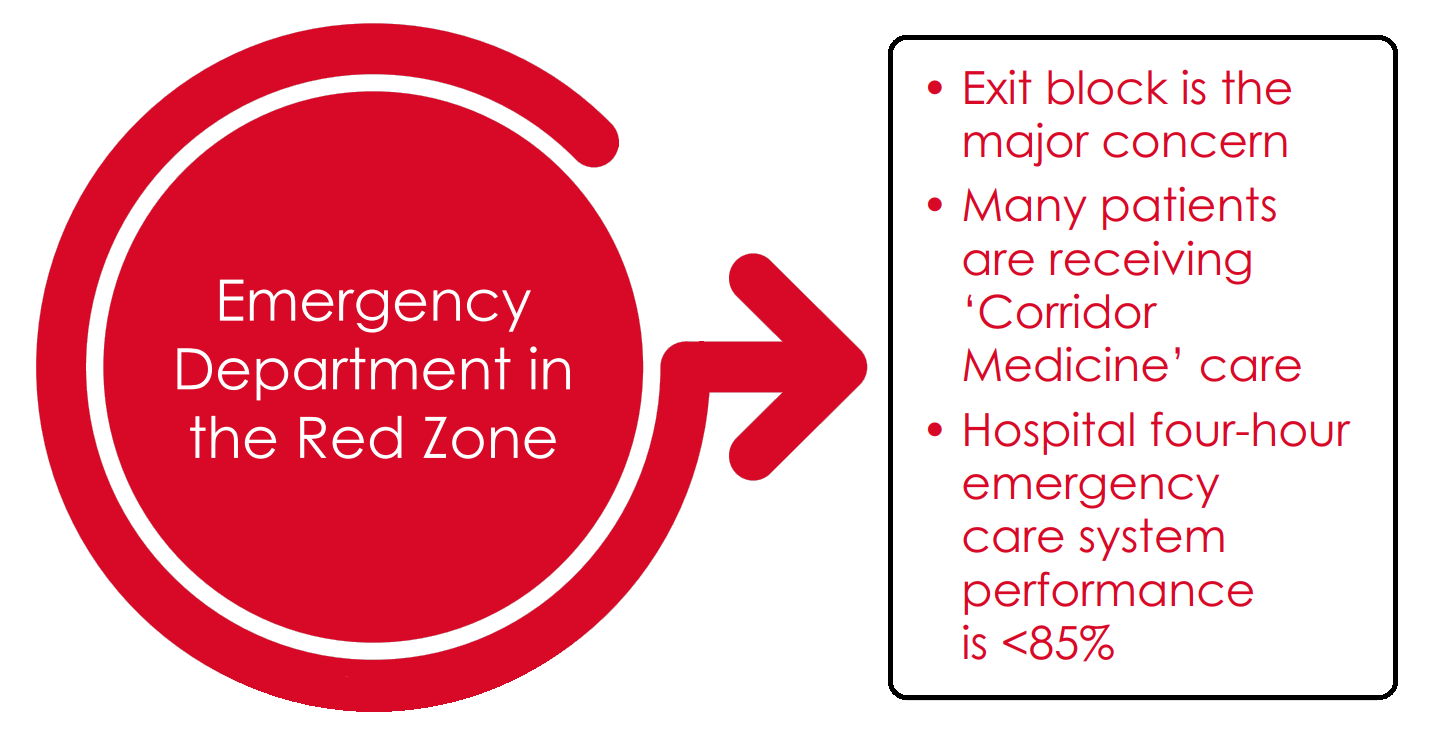
The guide below describes what systems should do, appropriate to the performance ‘zones’ EDs find themselves in; Green (4hr performance >95%), Amber (85-95%), or Red (<85%).
+ Where we are
In England

Improving safety in the Emergency Department this winter
RCEM Position Statement: Further Guidance on Winter Pressures – December 2018

+ Green Zone

Actions
1. How will you maintain safety, quality and dignity for patients in your crowded Emergency Department this winter?
2. What are your plans for safe staffing in your Emergency Department this winter in order to cope with demand?
3. What are your plans for safe staffing of assessment and escalation areas, medical wards and for ‘outliers’?
4. Does your hospital and system respond to demand in the evenings, at weekends and over holiday periods?
5. Is the wider system engaged to support achievement of the four-hour emergency care standard?
6. Is safety and performance against the four-hour standard at the highest level on your hospital risk register if your ED is in the Amber or Red Zone?
7. How will you value staff and maintain morale during periods of sustained pressure?